


When it seems like you've tried everything and still don't have any relief from your knee pain and debilitation, it may be time to consider knee replacement surgery. There are two different types of knee replacement procedures your doctor may recommend to relieve your knee pain, partial knee replacement, also called uni-compartmental replacement, or total knee replacement. Learning the differences can help you have a better discussion with your doctor. In knee replacement surgery, the ends of the bones that make up the knee are repaired. The new joint works the way cartilage works in a healthy knee by preventing the bones of the leg from rubbing together at the joint.
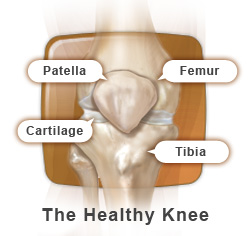
The knee is the largest joint in the body. It is commonly referred to as a “hinge” joint because it allows the knee to flex (bend) and extend. While hinges can only bend and straighten, the knee has the additional ability to rotate (turn) and translate (glide). The knee joint is formed by the tibia (shin bone), the femur (thigh bone) and the patella (knee cap). Each bone end is covered with a layer of smooth, shiny cartilage that cushions and protects while allowing near frictionless movement. Cartilage, which contains no nerve endings or blood supply, receives nutrients from the fluid contained within the joint.
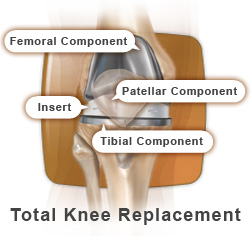
Total knee replacement, or arthroplasty, is the relining of the joint (bone end surfaces) with artificial parts called prostheses. There are three components used in the artificial knee. The femoral (thigh) component is made of metal and covers the end of the thigh bone. The tibial (shin bone) component, made of metal and polyethylene (medical-grade plastic), covers the top end of the tibia. The metal forms the base of this component, while the polyethylene is attached to the top of the metal to serve as a cushion and smooth gliding surface. The third component, the patella (kneecap) may be all polyethylene or a combination of metal and polyethylene. The new components are stabilized by your ligaments and muscles, just as your natural knee. In some cases, total knee replacement can be done through a smaller incision. This is called minimally invasive total knee replacement.
If X-ray and MRI (Magnetic Resonance Imaging) results tell us only one side of your knee is damaged, your surgeon may decide a partial knee replacement is right for you. Partial knee replacement repairs the side of the knee joint that is damage instead of the entire joint surface as in total knee replacement.
Because only one side of the knee is being replaced, a small incision may be used. Because of the small incision, this is sometimes referred to as “minimally invasive” surgery.
Partial knee replacement is not usually considered for active or heavy people because they can put too much stress on the implant. In addition, if two or more compartments of your knee are damaged, your surgeon will probably recommend total knee replacement.
The top of the shinbone is prepared in a similar way. The worn surface is removed, and a new metal tray is placed on top of the remaining bone. This tray holds a hard plastic spacer that will become the new shock absorber between the smooth metal coverings. Your surgeon may also replace the back of the kneecap with a new plastic surface.
Near the end of your surgery, your surgeon will attach the new metal and plastic coverings to the ends of the bones and the back of the kneecap. This can be done with bone cement where the new knee is essentially glued to the bones. This can also be done without cement with certain knee replacement implants that can be press-fitted tightly into the bones and affix to them naturally. Either way, your doctor wants to secure the new knee so you can get back on your feet as soon as possible. When the implant is in position and all of the supporting muscles and ligaments are working well, your surgeon closes the incision with stitches or staples.
When your surgery is over, you will be taken to the recovery room. A nurse will care for you and monitor your condition as your anesthesia wears off. You may experience some symptoms during this time such as blurry vision, dry mouth, nausea, chills, and perhaps some pain. If you do, let the nurse know so that they can provide you with medication to help ease your symptoms if appropriate. After recovering from the anesthesia, you will be asked to do some simple breathing and moving activities. These activities help to prevent possible post-surgical complications, such as developing blood clots in your legs. Generally, you can expect to be moved to your regular room within one to three hours after surgery.